Infected Mouth, What Does That Even Mean?
To say someone has an infected mouth is really more of a subjective description than a proper medical diagnosis. That’s because an oral infection could be many different things.
If you feel like there’s something strange happening with your lips, gums or teeth, or perhaps someone has told you that you have an infected mouth, then read on and let’s try and determine the specific problem. Perhaps you’re worried that you have perpetually bad breath, unsightly blemishes or chalky white bumps in your mouth? Let’s find the symptoms that most resemble your condition.
To say you have an infected mouth may just another way of saying you have chronic bad breath or visible mouth sores, or discomfort. This document lists many possibilities with pictures and descriptions. Your condition may just be an infected tooth which is sometimes called an abscessed tooth and which causes a pocket of smelly puss to form due to a bacterial infection. It’s usually caused by tooth decay, or maybe a physical mouth injury or previous dental work.
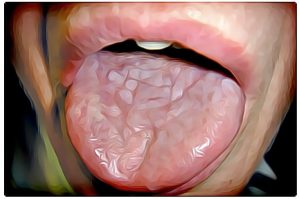
Yeast Infection in Mouth
Perhaps you have a yeast infection in your mouth? If that’s the case, then you suffer from a common condition called Candidiasis.


Oral thrush, or oral pseudomembranous candidiasis is a fungal infection that is a caused by a yeast, which is a type of fungus. Dentists and other oral health professionals call this oral thrush. The fungus appears as slightly raised removable plaques resembling cottage cheese on the tongue or inner cheek. It can also affect the roof of the mouth, gums, tonsils or back of the throat. The creamy white bumps can be scraped off which separates this from other conditions. It’s most common in infants and children, and when it occurs in adults it may be a sign of weakened immune system.
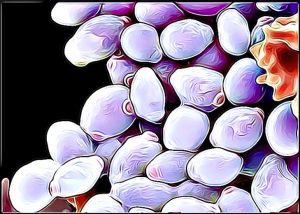
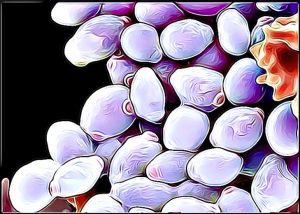
Candida is the name of the fungus and in normal conditions it’s almost always found in small amounts in the mouth and intestines. It’s only when it blooms out-of-control that it’s a problem. That’s Candidiasis, and it’s the most commonly occurring human fungal infection.
The afflicted person usually suffers dry mouth, high blood and salivary sugar levels (diabetes). The sufferer could experience some discomfort when chewing their food and a loss of taste, and they may even have difficulty swallowing. This is a yeast infection that develops on the inside of your mouth, and on your tongue.
The condition can be caused by prolonged use of certain antibiotics or asthma inhalers (corticosteroid therapy) which can upset the body’s natural balance of friendly bacteria that would otherwise fight off such a yeast infection. This lack-of-balance allows the overgrowth of Candida that leads to thrush.
What’s the remedy? Saltwater is the number one recommended solution. One tablespoon of salt in a glass of water has many antiseptic, cleansing, and soothing properties. Don’t swallow it. This makes it a common home rinse for many oral problems. Simply rinsing your mouth with saltwater could help relieve yeast build-ups. Probiotic yogurts, baking soda and lemon juice are also common remedies for oral thrush.
Meth Mouth Just Looks Infected!


Meth amphetamine contains chemicals that are corrosive. Meth labs explode when inexperienced criminals cook these substances. Exposing your teeth to the same chemicals will make them look infected. Anhydrous ammonia, phosphorus, and the same type of lithium that’s found in batteries are commonly found in meth. Excessive consumption of the drug allows these chemicals to destroy the coating of your teeth enamel.
Canker Sores and Cold Sores
Canker sores and cold sores are different things. Canker sores only occur in the soft tissues of the mouth, such as on your gums or inside your cheeks. Cold sores form on and around your lips, although in some cases they can also form inside your mouth. They’re caused by infection with the herpes simplex virus (HSV). Herpes labialis is a type of infection by the herpes simplex virus that affects primarily the lip. Symptoms typically include a burning pain followed by small blisters or sores. The first attack may also be accompanied by fever, sore throat, and enlarged lymph nodes.


Canker sores are also called aphthous stomatitis or aphthous ulcers. They’re small, painful, oval-shaped ulcers on the inside of the mouth that appear red, white, or yellow in color. These painful, fluid-filled blisters appear near the mouth and lips. Affected area will often tingle or burn before the sore is visible and sometimes prescient people can detect this feeling and react before ugly blemishes appear on the skin.
Outbreaks may also be accompanied by mild, flu-like symptoms such as low fever, body aches, and swollen lymph nodes. These symptoms are seldom life-threatening and this condition is usually harmless and the .
Recurrent ulcers may be a sign of other diseases, such as Crohn’s disease, celiac disease, vitamin deficiency, or HIV. But then let’s remember that mouth sores are common ailments that affect the majority of people at some point in their lives.


What’s the remedy? Occlusive medications are used to prevent external stimulation of the wound site and hold therapeutic agents such as Benzocaine or Boric Acid in place. Products in this category include Zilactin® and Zilactin®-B, Orajel®, and Orabase® Soothe-N-Seal™. Mouth sores, which include canker sores, are usually a minor irritation and will only last only a week or two. In some cases, however, they can indicate mouth cancer or an infection from a virus, such as herpes simplex. Archer Dental has penned a terrific blog post entitled Cures for Canker Sores which seems to be very popular reading in this country and around the world.
Adult Scurvy


What’s the difference between Anemia and Scurvy?
Scurvy is the name for a vitamin C deficiency that can lead to anemia which is a condition with symptoms that include debility, exhaustion, spontaneous bleeding, pain in the limbs, and especially the legs, swelling in some parts of the body, and sometimes ulceration of the gums and loss of teeth. The human body has to have vitamin C as the European sailors discovered in long sea voyages to the Americas. But there are other causes of anemia.
Anemia happens when a body’s red blood cells are so reduced, damaged, or impaired that you have problems transporting enough oxygen throughout your body. Symptoms include pale, cold skin, pale gums, dizziness, light-headedness, fatigue, increased or decreased blood pressure, and racing or pounding heart.
Anemia has many causes and may occur quickly (such as after an injury or surgery) or over a long period of time. Symptoms include fatigue, weakness, pale skin, fatigue, mouth sores, tongue swelling, and prematurely gray hair.
Folate-deficiency anemia is a decrease in red blood cells (anemia) due to a lack of folate. Folate is a type of B vitamin which the human body uses to make and repair DNA and it’s critical to proper neural tube development in embryos. It is also called folic acid. Anemia is a condition in which the body does not have enough healthy red blood cells. Folate is an important B vitamin and anemia, or low red blood cells, is the most common result of folate deficiency
What’s the remedy? Folate deficiency anemia is prevented and treated by eating a healthy diet. This includes foods rich in folic acid, such as nuts, leafy green vegetables, enriched breads and cereals, and fruit. Your doctor will also likely prescribe you a daily folic acid supplements. Vitamin C deficiency requires more citrus fruits and juices. Read Archer Dental blog post on The Dental Diet book by Dr. Steven Lin.
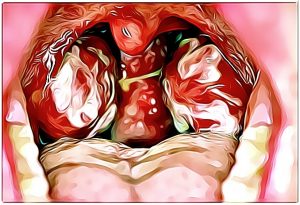
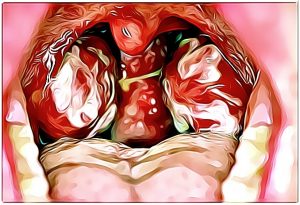
Gingivomatitis
Gingivostomatitis is a combination of gingivitis and stomatitis, or an inflammation of the oral mucosa and gingiva. Herpetic gingivostomatitis is often the initial presentation during the first or “primary” herpes simplex infection. It’s of greater severity than herpes labialis (cold sores) which is often the subsequent presentations. Primary herpetic gingivostomatitis is the most common viral infection of the mouth.


Gingivomatitis is a common infection of the mouth and gums, often seen in children. It produces tender sores on the gums or insides of cheeks; like canker sores, but they appear grayish or yellow on the periphery of the spot and red in the center.
It looks awful but it’s not especially dangerous. The also causes mild, flu-like symptoms and may lead to drooling and pain with eating, especially in young children
What’s the remedy? Most people find relief when they take medications prescribed by their doctor. Rinse your mouth with a medicated mouthwash containing hydrogen peroxide or xylocaine. These are readily available at your local drugstore. Eat a healthy diet. Avoid spicy, salty, or sour foods.
Infectious mononucleosis
Infectious mononucleosis is usually caused by the Epstein-Barr virus (EBV) can cause your mouth to look and smell absolutely terrible.
Epstein-Barr virus (EBV), also known as human herpesvirus 4, is a member of the herpes virus family. It is one of the most common human viruses. If anyone is interested, there are over one hundred known herpesviruses, but only eight routinely infect humans. EBV is not that dangerous but complications can arise especially in people with preexisting conditions.
Mono mainly occurs in high school and college students who exchange saliva while kissing. The best way to prevent infection is to avoid kissing or sharing dishes, food utensils, or personal items with anyone who has the sickness. Symptoms include fever, swollen lymph glands, sore throat, headache, fatigue, night sweats, and body aches.
What’s the remedy? It’s a sad fact that antibiotics don’t work against viral infections such as mononucleosis. The most effective treatment seems to be simply taking care of yourself and getting enough rest, eating a healthy diet and drinking plenty of fluids.
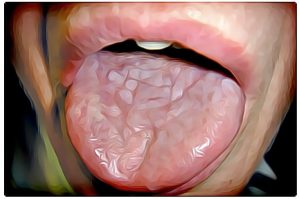
Leukoplakia
People suffering from Leukoplakia look like they have infected mouths.


Leukoplakia is a medical condition that causes white patches or spots (sometimes called lesions) to form inside the mouth. Leukoplakia is different from whitening ailments such as thrush or lichen planus because it can eventually develop into oral cancer.
Leukoplakia causes thick, white patches on your tongue and the lining of your mouth that may be raised, hard, or have a “hairy” appearance. It’s commonly seen in smokers. Regular dental care can help prevent recurrences.
Cancers on the bottom of the mouth can occur next to areas of leukoplakia. And white areas mixed in with red areas (speckled leukoplakia) may indicate the potential for cancer. So it’s best to see your dentist or primary care professional if you have unusual, persistent changes in your mouth.
One type of leukoplakia called hairy leukoplakia, and this primarily affects people whose immune systems have been weakened by EBV and other disease, especially HIV/AIDS.
What’s the remedy? See your dentist and get a professional cleaning and then use antiviral mouthwashes. People with HIV/AIDS are especially likely to develop hairy leukoplakia. The use of anti-retroviral drugs has reduced the number of cases, but hairy leukoplakia still affects a number of HIV-positive people, and it may be one of the first signs of HIV infection.
Oral lichen planus
Oral lichen planus is an ongoing (chronic) inflammatory condition that affects mucous membranes inside your mouth.
Oral lichen planus may appear as white, lacy patches combined with red, swollen tissues. Depending on severity the sufferer may also have open sores. These lesions may cause burning, pain or other discomfort and they would certainly cause someone to believe their mouth was infected.
This chronic inflammatory disorder affects the gums, lips, cheeks, and tongue. White, lacy, raised patches of tissue in the mouth resemble spiderwebs or tender, swollen patches that are bright red and may ulcerate. Open ulcers may bleed and cause pain when eating or brushing teeth.
Sometimes health professionals will take samples to help search for other factors. Tissue may be collected taken from one or more lesions in your mouth and examined under a microscope to look for indications. Other more specialized microscopic tests may be needed to identify immune system proteins. Or lab technicians can grow cultures. In this scenario a sample of cells is taken from your mouth using a cotton swab. The sample is examined under a microscope to determine whether you have a secondary fungal, bacterial or viral infection.
What’s the remedy? Oral lichen planus is a chronic condition. There is no cure, so the treatment focuses on helping severe lesions heal and reducing pain or other discomfort. Your doctor will monitor your condition to determine the appropriate treatment or stop treatment as necessary.
Celiac Disease


Celiac disease is an abnormal immune system’s response to gluten that damages the lining of the small intestine. Damage to the small intestine leads to poor absorption of important dietary nutrients like B vitamins, vitamin D, iron, and calcium.
Symptoms range in severity and may differ between adults and children. Adults often experience diarrhea, weight loss, stomach pain, anemia, joint pain, bloating, gas, fatty stools, skin rash, and mouth sores. Yellow or discoloured teeth are present in both adults and children with Celiac.
Celiac disease can cause tooth enamel defects and recurrent aphthous ulcers (canker sores). When dentists encounter these features, they should inquire about other clinical symptoms, associated disorders and family history of celiac disease. In suspected cases, the patient or family physician should be advised to obtain serologic screening for celiac disease and, if positive, confirmation of the diagnosis by intestinal biopsy. Dentists can play an important role in identifying people who may have unrecognized celiac disease. Appropriate referral and a timely diagnosis can help prevent serious complications of this disorder.
What’s the remedy? Once again there is no cure. The only treatment for celiac disease is to follow a gluten-free diet—that is, to avoid all foods that contain gluten. For most people, following this diet will stop symptoms, heal existing intestinal damage, and prevent further damage. Improvements begin within weeks of starting the diet.
Hand, Foot and Mouth Disease
Hand, foot and mouth disease is a mildly contagious viral infection common in young children. This ailment is characterized by sores in the mouth and a rash on the hands and feet. Hand-foot-and-mouth disease is most commonly caused by a coxsackievirus.


Coxsackieviruses are part of the enterovirus family of viruses (which also includes polioviruses and hepatitis A virus) that live in the human digestive tract. The viruses can spread from person to person, usually on unwashed hands and surfaces contaminated by feces (poop), where they can live for several days.
Afflicted people suddenly get a high fever, headache, and muscle aches, and some also develop sore throats and have abdominal discomfort or nausea. A child with a coxsackievirus infection may simply feel hot but have no other symptoms. In most kids, the fever lasts about 3 days, then disappears.
What’s the remedy? In most cases, coxsackievirus infections go away without treatment. But in some cases, they can lead to more serious infections. Depending on the type of infection and symptoms, the doctor may prescribe medicines to make your child feel more comfortable. Because antibiotics only work against bacteria, they can’t be used to fight a coxsackievirus infection.
Archer Dental’s Oral Health Professionals Are Dental Detectives


If you suspect there’s something wrong with your mouth, and if some of the medical conditions in the list conform to what you’re experiencing , please don’t hesitate to reach out and contact Archer Dental for an appointment.

